If you’re considering shockwave therapy for erectile dysfunction (ED), one of the first questions that often comes up is whether insurance will cover the treatment. The good news is that many PPO insurance plans, and now even Medicare, are beginning to reimburse qualified shockwave therapy procedures, making it easier for patients to access care with little to no out-of-pocket cost. However, proper documentation is essential to secure approval. Here’s what you need to know.
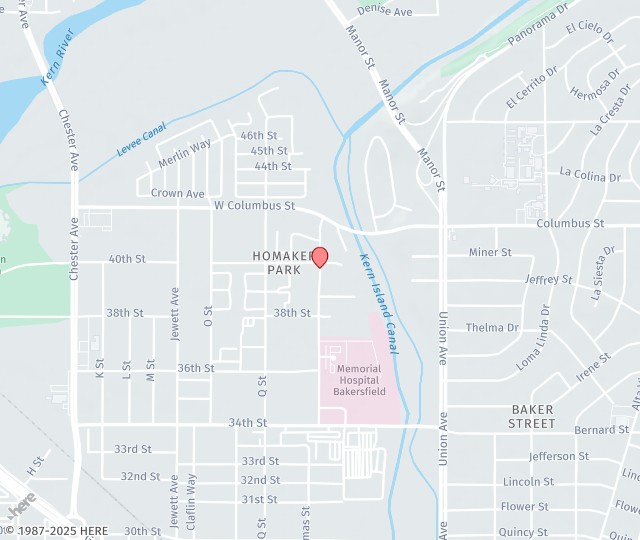
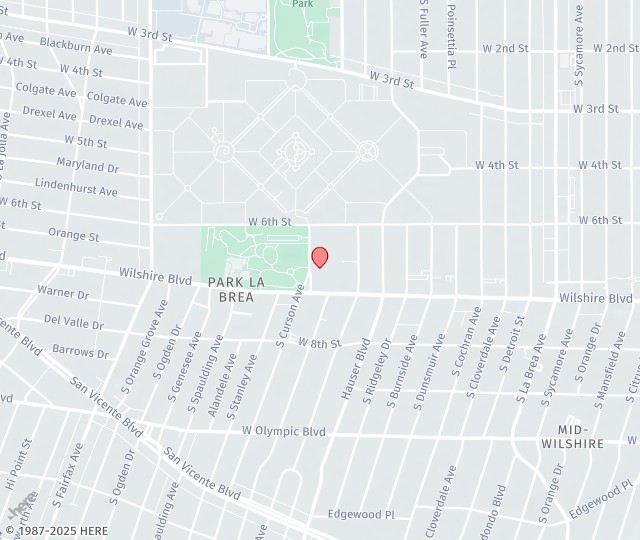
At Auxo Clinic, our nationally recognized urologists specialize in advanced, minimally invasive treatments for erectile dysfunction, including state-of-the-art shockwave therapy, in a warm, spa-like environment with locations in Los Angeles, San Diego, and Bakersfield.
Proof of Medical Necessity
Insurance providers want to see that shockwave therapy isn’t purely elective. To demonstrate medical necessity, your provider will typically need to submit:
- A detailed history of ED symptoms
- Duration and severity of the condition
- Previous treatments attempted
- Clinical notes supporting why shockwave therapy is the next appropriate step
This information helps insurers understand that ED is affecting your quality of life and requires medical guidance.
Diagnostic Test Results
Many insurance carriers require additional testing to confirm the underlying cause of ED. Common diagnostic materials may include:
- Penile Doppler ultrasound results
- Blood tests assessing hormone levels
- Cardiovascular evaluations, if needed
These tests give insurers a clearer picture of the condition and validate the need for advanced therapy.
Treatment Plan and Provider Notes
Your healthcare provider must submit a structured treatment plan outlining:
- The recommended number of shockwave sessions
- Device type and settings (if required by the insurer)
- Expected outcomes and goals
- Supporting clinical evidence that shockwave therapy is effective for your specific diagnosis
These details assure the insurer that the therapy is being administered appropriately and by a qualified provider.
Pre-Authorization Forms
Most insurers require pre-authorization before treatments begin. This includes:
- Insurance-specific request forms
- ICD-10 codes related to ED
- CPT codes associated with shockwave therapy (when applicable)
Submitting these forms accurately can prevent delays or denials.
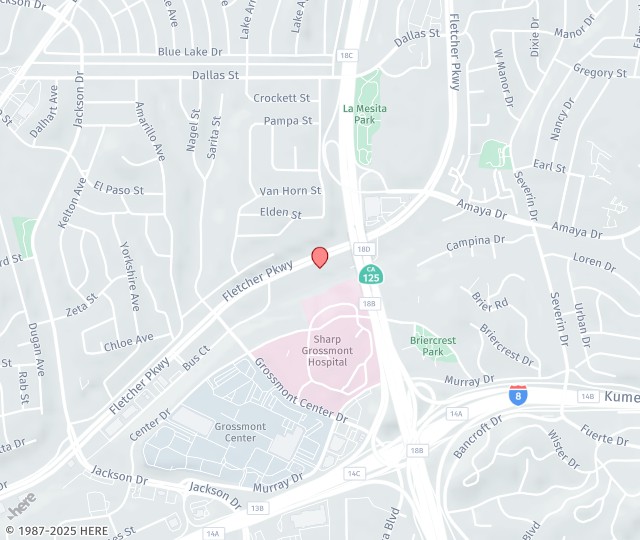
Treat Erectile Dysfunction with Insurance Coverage in Los Angeles, CA
Getting insurance approval for ED shockwave therapy is absolutely possible, especially with the right documentation. If you’re unsure where to start, your provider can help, making it easier to access the treatment you need. Call us today at 310-278-8330 in LA to schedule an appointment.